Columbia University
Irving Medical Center
Neurological Institute
710 West 168th Street, 3rd floor
(212) 305-1818
Featured Research
Celebrating Dr. Rafael Lantigua
» 14th ANNUAL TAUB INSTITUTE RESEARCH RETREAT, September 30, 2024
» 13th ANNUAL TAUB INSTITUTE RESEARCH RETREAT, November 8, 2023
» 12th ANNUAL TAUB INSTITUTE RESEARCH RETREAT, November 15, 2022
» Radhika Jagannathan, MD, PhD
» Taub Institute Grants: New in 2020
» ADRC Update: An Interview with Dr. Scott Small
» Chasing Therapeutics: From Neurodegeneration to Sars-CoV-2
» 10th ANNUAL TAUB INSTITUTE RESEARCH RETREAT, November 2019
» A Q&A with Brain Donation Coordinator Scott Reid
» Collaboratory on Research Definitions for Reserve and Resilience in Cognitive Aging and Dementia
» Center of Excellence for Alzheimer's Disease (CEAD) at Columbia University Irving Medical Center
» 9th ANNUAL TAUB INSTITUTE RESEARCH RETREAT, November 2018
» Columbia University Alzheimer's Disease Research Center (ADRC) 2018-19 Pilot Grant Awardees
» 8th ANNUAL TAUB INSTITUTE RESEARCH RETREAT, November 2017
» Qolamreza R. Razlighi, PhD: Quantitative Neuroimaging Laboratory
» Sandra Barral Rodriguez, PhD
» Catherine L. Clelland, MS, PhD
» 7th ANNUAL TAUB INSTITUTE RESEARCH RETREAT, October 2016
» Badri N. Vardarajan, PhD, MS
» Dr. Yaakov Stern: the Concept of Cognitive Reserve
» The Alzheimer's Disease Research Center at Columbia University Celebrates 25 Years
» Lawrence S. Honig, MD, PhD, FAAN
» 6th ANNUAL TAUB INSTITUTE RESEARCH RETREAT, October 2015
» Ismael Santa-Maria Perez, PhD
» 5th ANNUAL TAUB INSTITUTE RESEARCH RETREAT, October 2014
» Yaakov Stern, PhD: Cognitive Neuroscience of Aging Laboratory
» Michael Shelanski Laboratory
» Richard Mayeux, MD, MSc: Laboratory for Genetic Epidemiology
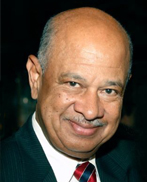
Rafael A. Lantigua, MD
After an incredible career devoted to research, education, and community service, Dr. Rafael Lantigua is retiring from Columbia to take on an exciting new role as Ambassador of the Dominican Republic to Rome!
For more than four decades, Dr. Lantigua has been a mentor, leader, and champion of community-based research, working to improve the health and well-being of aging minority populations. Since 1999, he has served as Deputy Director of the Taub Institute for Research on Alzheimer’s Disease and the Aging Brain, where he played a key role in advancing research on aging and neurodegenerative diseases, with a particular focus on minority populations.
Beyond his contributions to research, Dr. Lantigua has been a steadfast advocate for health equity, serving as Associate Dean for Community Service, Director of the Office of Community Service Programs, and Professor of Medicine at Columbia University Vagelos College of Physicians and Surgeons. His commitment to bridging academic medicine with community impact led to the creation of the Columbia Center for the Active Life of Minority Elders (CALME) and the Columbia Center for the Health of Urban Minorities, two initiatives that have deepened NYP/CUIMC’s engagement with the communities it serves.
While he may be stepping away from academia, his influence will continue to be felt in medicine, public service, and beyond. As he embarks on this new journey, we celebrate his exceptional career and wish him all the best in this next chapter. His legacy will continue to inspire, and we have no doubt he will bring the same dedication and passion to his diplomatic role. Congratulations, Dr. Lantigua!