Columbia University
Irving Medical Center
Neurological Institute
710 West 168th Street, 3rd floor
(212) 305-1818
Featured Research
In the Lab:
Nicole Schupf, PhD
 Nicole Schupf, PhD
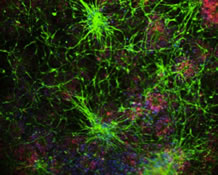
Nicole Schupf, PhDThe focus of my research is on studies of aging and Alzheimer's disease (AD) in adults with Down syndrome (DS), a population at high risk for AD. This work has been conducted in collaboration with Taub and CUMC colleagues Drs. Joseph Lee, Ben Tycko, and Jose Luchsinger, and with colleagues from the Kennedy Krieger Institute (Dr. Wayne Silverman) and the New York State Institute for Basic Research in Developmental Disabilities (Drs. Sharon Krinsky-Mchale, Warren Zigman, and Edmund Jenkins). Our studies include the relation of biomarker, genetic, and host factors to age-at-onset and risk of AD.
In addition, over the past 15 years, I have conducted studies of antecedent factors related to onset and risk of mild cognitive impairment (MCI) and AD in the community based Washington Heights Inwood Columbia Aging Project (WHICAP) cohort. I am a co-investigator on the WHICAP Study, Epidemiology of Biomarkers of Risk and Progression in Late Onset Alzheimer's Disease study, and was Core Leader of the Epidemiology, Database Management and Statistics Core for the WHICAP program project grant. I continue to work closely with Taub colleagues Drs. Richard Mayeux, Jennifer Manly, Adam Brickman, and Howard Andrews on the WHICAP study, to coordinate follow-up of the cohort, oversee linkage of laboratory data with clinical information, and consult with all investigators on data analysis. In addition, I am involved on studies of healthy aging and exceptional longevity, as co-investigator on the Long Life Family Study (LLFS), working with Taub colleagues Joseph Lee, Stephanie Cosentino, Sandra Barral, Lawrence Honig, Badri Vardarajan, and Giuseppe Tosto. Within this context, past and current projects include:
Biomarkers of Alzheimer's Disease in Adults with Down Syndrome
Many researchers believe that future Alzheimer's disease treatments may be most effective in the early stages of the disease, before the onset of symptoms and before irreversible neuron loss has occurred. This prospective study is part of an NIH initiative, Biomarkers of Alzheimer's Disease in Adults with Down Syndrome that supports two collaborative teams. Currently, I am the lead PI of one team at CUMC, with Dr. Ira Lott of the University of California, Irvine, Dr. Wayne Silverman of Kennedy Krieger Institute, Dr. Mei-Cheng Wang of Johns Hopkins University, Dr. Florence Lai and Diana Rosas of Massachusetts General Hospital/Harvard, Dr. Sharon Krinsky McHale of the New York State Institute for Basic Research in Developmental Disabilities, and Dr. Sid O’Bryant of the University of North Texas Health Sciences Center as the lead investigators at the additional sites. A second team is headed by Benjamin Handen, PhD, from the University of Pittsburgh. The study focuses on a longitudinal and multidisciplinary determination of key biomarkers that are likely to define the progression from normal aging to onset of dementia, including levels and rates of change in blood-based biomarkers such as beta-amyloid peptides, protein, inflammatory and lipid profiles, measures of amyloid and tau concentration in cerebrospinal fluid, neuroimaging-based changes, PET studies of brain amyloid uptake, and genetic polymorphisms. These biomarkers will be combined to develop the most valid indicators of preclinical and early stages of AD. The goal is to develop a noninvasive test to detect AD in individuals with DS and in the broader population. We are currently enrolling participants and conducting our assessments.
Familial Aggregation of Down Syndrome and Alzheimer's Disease (View Relevant Publications)
Age is the strongest risk factor for Alzheimer's disease. Most adults with Down syndrome develop neuropathology characteristic of AD by the age of 40. Most of the non-disjunction events in DS are of maternal origin. We hypothesized that a shared genetic susceptibility to DS and AD would be associated with an increased frequency of AD among mothers, but not fathers, of individuals with DS. We further hypothesized that the shared susceptibility could involve an accelerated aging process, leading to the birth of a child with DS to a relatively young mother and to an increased risk of dementia in mothers who were young when their child with DS was born compared with mothers who were older at the birth of a child with DS. The risk of dementia among mothers who were 35 or younger when their DS children were born was 5 times that control mothers, while there was no increase in risk of dementia among mothers who were older (> 35 years) at the proband's birth or among fathers.
Identifying Blood-Based Biomarkers of Risk in Alzheimer's Disease (View Relevant Publications)
Determining which individuals are at the highest risk can provide insights into AD pathogenesis, are critical to the early diagnosis of dementia, and can guide the development of effective intervention. Our biomarker studies, to date, have focused on the role of beta amyloid peptides in the pathogenesis of AD and their utility as a screening tool to identify high risk individuals and early detection of disease onset, and on AD-related genetic factors associated with individual differences in beta amyloid peptides.
Understanding the Role of Hormonal Risk Factors for Alzheimer's Disease (View Relevant Publications)
Among women with DS, younger age at menopause and lower levels of bioavailable estradiol in postmenopausal women were associated with a 3-4 fold increased risk of AD. In both women with DS and women in the general population, polymorphisms in genes involved in estrogen biosynthesis and in estrogen receptor activity were associated with earlier onset and an increased risk of AD. These findings support an important neuroprotective role for estrogen.
Healthy Aging and Longevity (View Relevant Publications)
The Long Life Family Study (LLFS) is a family study of longevity and exceptional survival traits among 546 families with multiple family members with long life spans. In population-based cohorts of the elderly, those with mild as well as severe cognitive impairment have been found to have an increased risk of death. Our group and others have documented a significant association between preserved cognitive function, successful aging and longevity. It is likely that cognitive traits, such as exceptional memory, might represent one of the several endophenotypes contributing to exceptional survival. In addition we have examined telomere length and extended maternal age as markers of exceptional longevity.
Nicole Schupf, PhD
Professor of Epidemiology (in Neurology, Psychiatry, the Gertrude H. Sergievsky Center, and the Taub Institute for Research on Alzheimer's Disease and the Aging Brain)
ns24@cumc.columbia.edu