Columbia University
Irving Medical Center
Neurological Institute
710 West 168th Street, 3rd floor
(212) 305-1818
Featured Research
Clinical Research:
Edward D. Huey, MD
 Edward D. Huey, MD
Edward D. Huey, MDDr. Edward (Ted) Huey is board-certified in adult psychiatry and neuropsychiatry. He specializes in the interface between Neurology and Psychiatry. In his work, Dr. Huey seeks to incorporate the best of both traditions: the rigorous brain localization and measurement of cognition of Neurology with the detailed and reliable Psychiatric assessment of behavior and emotion. In the Taub Institute, Dr. Huey investigates the neurological causes of psychiatric Illness and the causes of psychiatric symptoms in patients with neurological disorders.
Specifically, Dr. Huey has four main areas of interest:
1. Understanding the neuroanatomy and mechanisms underlying the behavioral, emotional, and cognitive symptoms of non-Alzheimer's dementias (especially FTD) and brain injury. Dr. Huey works mostly with patients with Frontotemporal dementia (FTD), but also with patients with Huntington's disease, FTD-ALS (amyotrophic lateral sclerosis), Corticobasal syndrome, and Traumatic Brain Injury. He has demonstrated that specific regions of the frontal lobes are associated with specific executive functions, and that the frontal and parietal cortexes have differential functions in praxis. He and colleagues have shown that social semantic knowledge appears to be selectively stored in the anterior temporal lobes and that specific brain regions are associated with apathy and awareness of symptoms in neurodegenerative disorders. He recently demonstrated that specific patterns of visuospatial dysfunction are associated with Corticobasal syndrome (CBS) caused by Alzheimer's disease vs. CBS caused by Corticobasal ganglionic degeneration (CBGD). Dr. Huey is interested in learning more about the mechanisms of frontal lobe functions by working with patients with frontal lobe dysfunction.
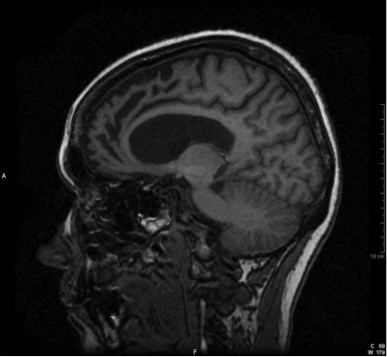
MRI of a patient suffering from Frontotemporal dementia (FTD)
2. Investigating the genetic bases and phenotypes of FTD. Dr. Huey was the first to describe the most common mutation in the GRN gene that causes FTD. Until the C9ORF72 mutation was recently discovered, this was the most common mutation known to cause FTD. He was the first to report that mutations that cause FTD can also result in the phenotype of schizophrenia, an association which has since been replicated and expanded by several other groups. This was the first time a single mutation has been shown to result in the phenotype of schizophrenia. Dr. Huey and colleagues have described the clinical and pathological presentation of FTD patients with mutations in MAPT, GRN, CHMP2B, FUS, and C9ORF72 and developed algorithms for clinical genetic testing in FTD. He is currently NIH-funded to examine the earliest phenotypic and biomarker changes that occur in familial FTD.
3. Developing and testing treatments for FTD. Dr. Huey has written several reviews of the neurotransmitter deficits associated with FTD and related illnesses, the effect of neurotransmitter-based medications used to attempt to reduce symptoms, potential future directions for drug development for FTD, and non-pharmacologic treatments for FTD and related illnesses. He has performed trials on direct current electrical stimulation of the cortex, and the use of dopaminergic medications, to treat symptoms of FTD. Dr. Huey recently completed a trial testing the effects of frontal dopamine augmentation in FTD, and is currently running a multi-center trial on medications to reduce agitation in FTD.
4. Applying the lessons learned from 1, 2, and 3 above to better understand the neuroanatomical, genetic, and neurotransmitter bases of psychiatric disorders. Dr. Huey has demonstrated that, in patients with penetrating brain injury, damage to the limbic system, including the ventromedial prefrontal cortex, is associated with a decreased incidence of anxiety disorders, depressive symptoms, and an increased incidence of externalizing psychiatric symptoms (e.g., substance abuse, aggression). These findings suggest that the ventromedial prefrontal cortex plays an important role in the subjective perception of anxiety and dysphoria and the regulation of social behaviors. He has explored the prevalence and pathogenesis of psychiatric disorders in neurological illnesses such as ALS and Essential Tremor and explored the neuroanatomical bases of pseudobulbar affect.
 From left to right, Gayathri Cheran, Masood Manoochehri, Jill Goldman, and Ted Huey.
|
Members of Dr. Huey's research team include:
Jill S. Goldman, MS, MPhil, CGC. Jill is a genetic counselor with expertise in FTD and other neurodegenerative disorders, in addition to the genetics of neurological disorders, more generally. She is the genetic counselor for the Columbia Huntington's Disease Society of America Center of Excellence. She is interested in algorithms for genetic testing, the range of phenotypes associated with mutations that cause FTD, especially C9ORF72, assessment of genetic risk, and education in genetics and genetic counseling. She runs several support groups for patients with neurodegenerative disease and their caregivers.
Masood Manoochehri, BA. Masood is the coordinator of the ARTFL and LEFFTDS studies. These are multi-site studies designed to assess the biological (blood, CSF, MRI) and phenotypic changes associated with mutations that cause FTD including C9ORF72, GRN, and MAPT, and to establish a treatment registry for patients with FTD. Subjects include mutation carriers, non-carriers, symptomatic and asymptomatic subjects. Masood also has coordinated clinical treatment trials for FTD and works on clinical research with patients with Huntington’s disease.
Gayathri Cheran, BS. Gayathri coordinates a NIH-funded study to characterize the course of familial FTD caused by mutations in the MAPT gene. She works closely with symptomatic and asymptomatic members of families with MAPT mutations to collect biological (MRI, blood, CSF, tau PET imaging) and behavioral and cognitive data to determine the biological and phenotype course of pre-symptomatic and symptomatic FTD.

