Columbia University
Irving Medical Center
Neurological Institute
710 West 168th Street, 3rd floor
(212) 305-1818
TaubCONNECT Research Perspectives:
September 2018
2: » Evaluation of TDP-43 Proteinopathy and Hippocampal Sclerosis in Relation to APOE ε4 Haplotype Status: A Community-Based Cohort Study
» #1 A Multi-Omic Atlas of the Human Frontal Cortex for Aging and Alzheimer's Disease Research
» #2 Whole-exome Sequencing in 20,197 Persons for Rare Variants in Alzheimer's Disease
» #2 Medical Retirement from Sport after Concussions: A Practical Guide for a Difficult Discussion
» #1 Cross Domain Self-Monitoring in Anosognosia for Memory Loss in Alzheimer's Disease
» #2 White Matter Changes in Alzheimer's Disease: A Focus on Myelin and Oligodendrocytes
» #1 ZCCHC17 is a Master Regulator of Synaptic Gene Expression in Alzheimer's Disease
» #2 Imaging Translocator Protein as a Biomarker of Neuroinflammation in Dementia
» #3 A Transcriptomic Atlas of Aged Human Microglia
» #1 Neuronal Lysosomal Dysfunction Releases Exosomes Harboring APP C-terminal Fragments and Unique Lipid Signatures
» #1 Neuronal Hyperactivity Due to Loss of Inhibitory Tone in APOE4 Mice Lacking Alzheimer's Disease-Like Pathology
and
» The Endosomal–Lysosomal Pathway Is Dysregulated by APOE4 Expression in Vivo
» First Place: A CSF Proteomic Screen Links Retromer to Alzheimer's Pathogenic Pathways and Suggests Endosomal-Trafficking Biomarkers
» First Place: Microglia Identity in the Aged and AD Human Brain
» #1 Intra-Axonal Synthesis of SNAP25 is Required for the Formation of Presynaptic Terminals
» #1 Stabilization of Dynamic Microtubules by mDia1 Drives Tau-dependent Aβ1-42 Synaptotoxicity
» #2 LTP and Memory Impairment Caused by Extracellular Aβ and Tau Oligomers is APP-Dependent
» #2 Neuropathologic Features of TOMM40 '523 Variant on Late-Life Cognitive Decline
» #2 An Approach to Studying the Neural Correlates of Reserve
» #1 Brain Atrophy Can Introduce Age-Related Differences in BOLD Response
» #2 Age-Related Biomarkers in LLFS Families With Exceptional Cognitive Abilities
» #2 Polygenic Risk Scores in Familial Alzheimer Diseases
» #1 Local Synthesis of Dynein Cofactors Matches Retrograde Transport to Acutely Changing Demands
» #3 Relation of Dysglycemia to Structural Brain Changes in a Multiethnic Elderly Cohort
 |  |
| Giuseppe Tosto, MD, PhD | Richard Mayeux, MD, MSc |
While autopsy remains the "gold standard" for a definitive diagnosis of Alzheimer's disease (AD), elevated levels of total tau (tTau), 181-phosphorylated phosphorylated tau (pTau), and decreasing levels of amyloid-β42 (Aβ42) in antemortem lumbar cerebrospinal fluid (CSF) have been associated with AD and correlated with postmortem amyloid plaque load. In 2014, a consensus was reached by the Alzheimer’s Biomarkers Standardization Initiative (ABSI) that lumbar puncture CSF biomarker analysis should be considered as a routine clinical test in patients referred for memory complaints or admitted to hospitals for cognitive impairment and complex differential diagnoses of dementia. However, most published studies on these CSF biomarkers in the diagnosis of AD have been from research settings that compared AD patients to healthy controls.
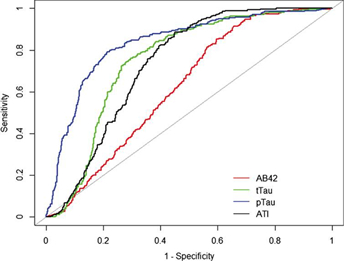
Figure: Receiver operation curve (ROC). Alzheimer's disease compared to overall population of the cohort. Alzheimer's disease (n = 264) was compared to the overall population of the cohort (n = 752). Aβ42 (red), tTau (green), pTau (blue), and ATI (black) CSF biomarker ROC curves are reported here. AUC analyses fully reported in the text.
Thus, in the present study, Drs. Richard Mayeux, Giuseppe Tosto, Larry Honig, Andy Teich, and colleagues sought to provide a realistic and unbiased evaluation of these CSF biomarkers in a non-research setting, by assessing the sensitivity, specificity, and area under the curve (see figure) of CSF Aβ42, tTau, pTau, and the Aβ42/total tau index (ATI) from the medical records of 1,016 patients that had CSF studies for dementia over a 12-year period at NewYork-Presbyterian/Columbia University Irving Medical. As published in the Journal of Alzheimer's Disease, their results indicate that, individually, CSF biomarkers Aβ42, tTau, pTau, and the computed ATI provide excellent sensitivity but moderate to low specificity for clinically diagnosed AD compared to patients with other diseases or other forms of dementia in routine practice. The use of CSF biomarkers in the diagnosis of patients meeting the clinical criteria listed by ABSI needs to be state of the art in identifying AD; the findings presented here indicate that further work needs to be done to improve their specificity and overall accuracy.
Giuseppe Tosto, MD, PhD
Postdoctoral Research Scientist (in the Taub Institute and the Gertrude H. Sergievsky Center)
gt2260@cumc.columbia.edu
Richard Mayeux, MD, MSc
Gertrude H. Sergievsky Professor of Neurology, Psychiatry and Epidemiology (in the Gertrude H. Sergievsky Center and in the Taub Institute)
rpm2@cumc.columbia.edu

Philip De Jager, MD, PhD, MMSc
Transactive response DNA-binding protein of 43 kDa (TDP-43) proteinopathy in older adults frequently coexists with Alzheimer's disease pathology and hippocampal sclerosis. It is unclear whether there is a link between APOEε4 and TDP-43 proteinopathy, and the role of APOEε4 in the association of TDP-43 proteinopathy with hippocampal sclerosis remains to be examined. According to a new study by Dr. Philip De Jager and colleagues, genetic association studies can provide a unique opportunity to examine the relationship between different post-mortem neuropathologies by assessing shared genetic associations between two pathologies.
As published in The Lancet Neurology, Dr. De Jager and colleagues leveraged the largest TDP-43 proteinopathy dataset reported, to date, to investigate the relationships among Alzheimer's disease, TDP-43 proteinopathy, and hippocampal sclerosis through a shared genetic risk factor, APOE ε4. In this study of more than 1000 well-characterized older adults from the Religious Orders Study (ROS) and the Rush Memory and Aging Project (MAP) community-based cohorts, they found that APOE ε4 is a strong genetic predictor of the presence and severity of TDP-43 proteinopathy, and this effect, in turn, was associated with higher odds of hippocampal sclerosis, a pathology potentially downstream of TDP-43 proteinopathy.. This association was not fully explained or significantly moderated by other APOE ε4-related proteinopathies. The authors conclude that TDP-43 proteinopathy contributes to the detrimental effect of APOE ε4 on late-life cognition through mechanisms independent of Alzheimer's disease pathology, and future research should consider that TDP-43 proteinopathy might be an integral component of APOE-related neurodegeneration.
Philip De Jager, MD, PhD, MMSc
Weil-Granat Professor of Neurology (in the Taub Institute, the Precision Medicine Initiative, and the Center for Translational and Computational Neuro-immunology)
pld2115@cumc.columbia.edu

