Columbia University
Irving Medical Center
Neurological Institute
710 West 168th Street, 3rd floor
(212) 305-1818
TaubCONNECT Research Perspectives:
April 2018
2: » Medical Retirement from Sport after Concussions: A Practical Guide for a Difficult Discussion

Scott Small, MD
The relevance of the retromer complex to the pathophysiology of Alzheimer's disease (AD) was first established by Taub Institute investigators Drs. Scott Small and Tae Wan Kim, using a molecular profiling study that relied on functional imaging observations in patients and animal models to guide its molecular analysis (Small et al., 2005). Since that time, there has been a veritable explosion of research focused on a causal role for the retromer and the specific molecular mechanisms by which the retromer affects amyloid precursor protein (APP) processing. Deficiencies in retromer-mediated transport have since been implicated not only in AD, but also in Parkinson's disease and Down syndrome (DS), as well as other non-neurological conditions. Most recently, studies have shown that retromer is a tractable target in drug discovery for these and other disorders of the nervous system (Small and Petsko, 2015).
In 2014, the Small laboratory,working together with Drs. Greg Petsko and Dagmar Ringe, identified a new family of small molecules that appeared to stabilize the interaction between members of the retromer complex and enhance its function in neurons: the retromer pharmacological chaperones (Mecozzi et al., 2014). These molecules, R33 and R55, increased flow through the endosome andreduced Aβ in mouse hippocampal neurons in a retromer-dependent manner, suggesting their potential as therapeutics for neurological disorders (Berman et al., 2015). However, to move forward in investigation of therapeutic strategies for humans, it is critical to test candidates in a human-specific system. In addition, how retromer stabilization affects components of the disease process other than Aβ, such as TAU hyperphosphorylation, and whether these two events are interdependent, is unknown.
Thus, Dr. Small teamed up with Drs. Jessica Young (University of Washington) and Lawrence S. B. Goldstein (University of California, San Diego) to extend these studies using hiPSC-derived neurons from sporadic AD (SAD) and familial AD (FAD) patients and from genome-edited hiPSC lines. This allowed the investigators to modulate the amounts of Aβ generation and APP expression in neurons and test how retromer stabilization by the small molecule chaperone R33 affects endogenous levels of Aβ and phospho-TAU (pTAU) in a human-specific system. Developing methods of improving endocytic trafficking and function in multiple CNS types will likely be protective in many neurodegenerative disorders, underscoring the importance of elucidating the role of the endocytic network in both Aβ and TAU pathology.
As published in Stem Cell Reports, Dr. Small and colleagues replicated work previously published in mice to show that retromer stabilization decreases pathogenic APP processing (Mecozzi et al., 2014) and extended these studies to show a beneficial effect of retromer stabilization on TAU in human neurons. Further, they demonstrate that this process correlates with, but is not dependent upon, APP processing. Indeed, these findings appear to support the "dual pathway" hypothesis, where an upstream molecular driver influences Aβ and TAU pathologies separately (Small and Duff, 2008). This may especially be the case for SAD, where immense genetic heterogeneity and complex environmental interactions have unknown influences on the course of the disease. Here, Young et al. conclude that "using hiPSCs, both from patients and isogenic lines with key mutations or variants, to test and screen novel therapeutic molecules and other therapeutic strategies will represent a major advance in therapeutic development for AD and other complex neurodegenerative disorders."
Scott Small, MD
Boris and Rose Katz Professor of Neurology
sas68@cumc.columbia.edu
Medical Retirement from Sport after Concussions: A Practical Guide for a Difficult Discussion

James M. Noble, MD, MS, CPH
Since 2011, neurologist and Taub Institute faculty member Dr. James Noble has been steadily building an impressive clinical and research program in Concussion and Sport-Related Head Injury at Columbia. Dr. Noble serves as a clinician for both amateur and professional athletes, a member of the Medical Advisory Board of the New York State Athletic Commission, and an investigator in the Big Ten/Ivy League Traumatic Brain Injury Research Collaboration. He has been particularly focused on addressing the fundamental problem of athletes failing to get diagnosed for concussion. As a result, Dr. Noble, in partnership with Dr. Barclay Morrison (Columbia Biomedical Engineering) and with help from the Columbia-Coulter Translational Research Partnership, developed a prototype football helmet equipped with EEG leads and sensors that uses a novel algorithm to detect concussions in real time and send a signal to a monitoring device on the sidelines, as reported by CUMC Newsroom and WIRED magazine.
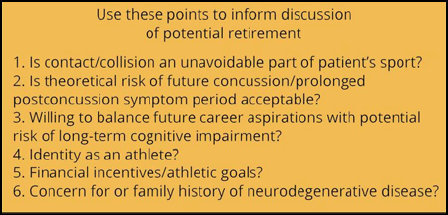
More recently, Dr. Noble turned his attention toward the relatively unchartered, thorny area of how and when to initiate difficult discussions of medical retirement in patients with a considerable history of sports-related concussion (SRC). The decision to retire a player often rests on a combination of many relative factors, which lack evidence-based support and can be difficult to navigate. Working in collaboration with the Department of Orthopedic Surgery, Dr. Noble drew from the group’s combined experience treating thousands of SRC patients to create a novel treatment algorithm—the Columbia SRC Retirement Algorithm—to guide clinicians through consideration of medical retirement following concussion. Published recently in Neurology Clinical Practice, with first authors Drs. Cecilia Davis-Hayes and David Baker (former P&S medical students), this provider decision algorithm includes 10 illustrative vignettes of high-risk athletes, which cover a wide range of ages, sports, and competitive levels, and highlight key points in conducting a retirement discussion, even in the absence of an absolute contraindication to return to sport.
James M. Noble, MD, MS, CPH
Assistant Professor of Neurology at CUMC
jn2054@cumc.columbia.edu

