Columbia University
Irving Medical Center
Neurological Institute
710 West 168th Street, 3rd floor
(212) 305-1818
TaubCONNECT Research Perspective:
December 2025
2: Elevated Expression of the Retrotransposon LINE-1 Drives Alzheimer's Disease-Associated Microglial Dysfunction
3: "Rest of the Folks are Tired and Weary": The Impact of Historical Lynchings on Biological and Cognitive Health for Older Adults Racialized as Black
 |  | |
| Wudu Lado, PhD | Ahrom Ham, PhD | |

|  | |
| Hongyu Li, PhD | Guomei Tang, PhD |
Synaptic and Cognitive Impairment Associated with L444P Heterozygous Glucocerebrosidase Mutation
Cognitive impairment is a prevalent yet insufficiently understood non-motor feature of Parkinson's disease (PD), significantly reducing patients' functional abilities and quality of life. The underlying mechanisms of cognitive decline in PD remain unclear, hindering effective prevention and treatment approaches. To address this knowledge gap, our team, including co-first authors Wudu Lado, Ahrom Ham, and Hongyu Li, explored the molecular and cellular processes contributing to cognitive impairment linked to heterozygous mutations in GBA1, the primary genetic risk factor for PD.
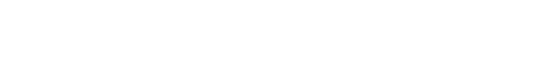
Figure 1. Mutations in GBA1 are the strongest genetic risk factor for Parkinson's disease. Lado et al report that GBA1 mutation perturbs hippocampal synaptic structure and function and causes cognitive impairment without motor deficits. When ╬▒-synuclein overexpression, this mutation synergizes with ╬▒Syn pathology, accelerating cognitive decline and motor symptoms associated with Parkinson's disease
GBA1 encodes glucocerebrosidase (GCase), a lysosomal enzyme responsible for breaking down glucosylceramide into glucose and ceramide. As recently reported in BRAIN, in collaboration with the laboratories of Drs. Serge Przedborski, Arancio Ottavio, and Roy Alcalay, we utilized the Gba1L444P/+ mouse model to demonstrate that the heterozygous L444P Gba1 mutation (L444P/+) induces deficits in hippocampus-dependent spatial and reference memory. These effects occur independently of ╬▒-synuclein (╬▒Syn) aggregation, lipid substrate accumulation of GCase, dopaminergic dysfunction, or motor impairments. The mutation impairs hippocampal synaptic plasticity and basal synaptic transmission by reducing the density of CA3-CA1 synapses in the hippocampus, a process that is distinct from ╬▒Syn-driven presynaptic neurotransmitter release dysfunction.
In a Thy1-╬▒Syn pre-symptomatic PD mouse model, which overexpresses human ╬▒Syn, we observed that the L444P/+ mutation intensifies hippocampal ╬▒Syn accumulation, synaptic abnormalities, and cognitive deficits in young double mutant Gba1L444P/+:Thy1-╬▒Syn mice. As the Thy1-╬▒Syn mice age, motor impairments emerge, and double mutant mice experience more severe synaptic and motor impairments compared to Thy1-╬▒Syn mice alone.
Taken together, our findings indicate that the heterozygous L444P GBA1 mutation disrupts hippocampal synaptic structure and function, contributing to a subclinical burden for cognitive impairment. When coupled with ╬▒Syn overexpression, this mutation synergizes with ╬▒Syn pathology, accelerating cognitive decline and motor symptoms associated with Parkinson's disease.
Guomei Tang, PhD
Assistant Professor of Neurological Sciences (in Neurology)
gt2107@cumc.columbia.edu
 |  |  | ||
| Nainika Roy, PhD | Jason C. Ngo | Falak Sher, PhD |
Transposable elements, once dismissed as "junk DNA," are now recognized as critical regulators of cellular function and dysfunction. Among these, long interspersed nuclear element-1 (LINE-1) is the most abundant retrotransposon in the human genome, comprising approximately 17% of our DNA. LINE-1 activity is typically suppressed in healthy cells, but aging and pathological states, such as AlzheimerÔÇÖs disease (AD), can lead to its aberrant activation. This dysregulation raises fascinating questions about the role of LINE-1 in brain aging and neurodegeneration, making it a promising target for research into mechanisms underlying AD.
-Representative-images.jpg)
Figure. (A) Representative images showing LINE-1 ORF1p (red) protein expression in neurons (NeuN), microglia (IBA1), oligodendrocytes (CNPase), and astrocytes (GFAP) in dorsolateral prefrontal cortex (DLPFC) of an aged human brain. (B) Representative images of microglia and LINE-1 (ORF1p) staining in postmortem brain tissues from cognitively healthy controls (C) and LOAD patients, highlighting microglial morphology and LINE-1 activity. Scale bars: 10 ┬Ám.
In a study spearheaded by recent PhD graduate Dr. Nainika Roy, my laboratory explored the role of elevated LINE-1 activity in microglial dysfunction associated with late-onset AlzheimerÔÇÖs disease (LOAD). Published in Acta Neuropathologica, our research utilized human postmortem brain tissue and a next-generation CRISPR-activation system in iPSC-derived microglia to uncover a significant link between heightened LINE-1 expression and disease-relevant microglial changes. These changes include impaired phagocytosis of amyloid-beta, altered cytokine secretion, and disrupted lipid metabolismÔÇökey processes essential for preserving brain health. Our findings highlight aberrant LINE-1 activity as a potential driver of microglial dysfunction and a contributing factor to AlzheimerÔÇÖs disease pathogenesis.
This study highlights the underappreciated role of LINE-1 in neurodegenerative processes and opens new avenues for therapeutic interventions. By targeting LINE-1 activity, we may uncover novel strategies to mitigate neuroinflammation and restore microglial function in AlzheimerÔÇÖs disease. This work reflects the innovative approaches pursued at TAUB Institute to advance the understanding of complex brain disorders and translate these insights into actionable treatments.
Falak Sher, PhD
Assistant Professor of Neurological Sciences (in Neurology and in the Taub Institute)
fs2644@cumc.columbia.edu
 |
 |
Paris Adkins-Jackson, PhD, MPH | Jennifer J. Manly, PhD |
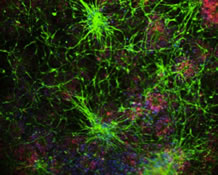
Our recent publication in Social Science and Medicine estimates the association between a common experience of modern older adults, historical lynchings, and markers for AlzheimerÔÇÖs disease risk like poor cognitive performance and elevated systemic inflammation (via C-reactive protein). This study began as an exploration of common historical experiences that modern older adults lived through. For many marginalized groups, lynchings are not a distant historical event. A lynching is the murder of individual by another individual or group based on racial prejudice. This act was most often committed by people racialized as White towards people racialized as Black following the Emancipation Proclamation through to the present.
Previous literature on lynchings suggests most occurred between 1882-1968, which means modern older adults racialized as Black might have experienced this phenomenon or grew up hearing about it. With this premise, and our earlier studies that suggest both before birth and early life exposures play a role in cognitive decline, we explored the association of historical lynchings between 1882-1968 with cognitive performance and systemic inflammation in mid-late life.
Our findings suggest adults racialized as Black experience greater systemic inflammation and lower cognitive performance in mid-late life when they live in states where a greater proportion of people racialized as Black were lynched between 1882-1968, compared to participants living in states with lower proportions of lynchings. This relationship demonstrates the link between historical experiences and mid-late life health consequences for modern older adults.
Paris Adkins-Jackson, PhD, MPH
Assistant Professor of Epidemiology and Sociomedical Sciences
pa2629@cumc.columbia.edu
Jennifer J. Manly, PhD
Professor of Neuropsychology (in Neurology, the Sergievsky Center, and the Taub Institute)
jjm71@cumc.columbia.edu