Columbia University
Irving Medical Center
Neurological Institute
710 West 168th Street, 3rd floor
(212) 305-1818
TaubCONNECT Research Perspectives:
August 2021
2: Midlife Vascular Factors and Prevalence of Mild Cognitive Impairment in Late-Life in Mexico
3: Effect of Aerobic Exercise on White Matter Tract Microstructure in Young and Middle-Aged Healthy Adults
 |
| Stephanie Cosentino, PhD |
Neuropsychological tests are a key component of diagnosing Alzheimer’s disease (AD), teasing apart typical age-related changes from those associated with degenerative disease. As a reflection of the underlying regional neuropathology, individual neuropsychological tests may hold prognostic value for disease progression, including time to specific disease outcomes. Previous work in a highly educated, predominantly Non-Hispanic White, clinic-based cohort showed that global cognition, orientation, and memory scores best predicted severe dependency. Little is known about whether these findings would be similar among Hispanics, an ethnic group disproportionately affected by AD.
In the current study, we assessed the differential utility of various neuropsychological tests for predicting severe dependency in a cohort of individuals from the Predictors 3 study, an ongoing study examining heterogeneity in disease course and outcomes among individuals with AD. Predictors 3 participants are drawn from the multiethnic, community-based cohort of elders residing in Northern Manhattan and enrolled in the Washington Heights-Hamilton Heights-Inwood Columbia Aging Project (WHICAP). As recently reported in the Journal of Alzheimer’s Disease, we found that relatively preserved semantic and memory abilities, as opposed to reasoning and spatial function, were associated with a reduction in risk of severe dependency. Specifically, higher scores on a list learning test, and measures of semantic knowledge including object naming and category fluency predicted a reduction in the risk of severe dependency (Naming (hazard ratio (HR 1) =0.90, p=0.036), Category Fluency (HR1=0.83, p<0.001), Delayed List Recall (HR1=0.81, p=0.044), and List Recognition (HR1=0.88, p=0.011).
From a clinical standpoint, it is informative to compare the effect of these cognitive scores to that of age on the risk for severe dependency. In our study, a one-year increase in age had a HR of 1.04, such that for every year older at baseline, individuals had a 4% higher chance of developing severe dependency. In comparison, for each one-point increase in naming scores, there was a 10% reduction in risk of developing severe dependency, similar to the magnitude of risk reduction for being 2.5 years younger at baseline. These results are consistent with the literature demonstrating that both semantic processing and memory can help predict the progression of AD, and extend knowledge regarding these predictors to a multiethnic community cohort.
Stephanie Cosentino, PhD
Associate Professor of Neuropsychology Associate Professor of Neuropsychology (in Neurology, the Gertrude H. Sergievsky Center, and the Taub Institute)
sc2460@cumc.columbia.edu
Midlife Vascular Factors and Prevalence of Mild Cognitive Impairment in Late-Life in Mexico
 |  |  | ||
| Miguel Arce RenterÃa, PhD | Sandra Barral, PhD | Giuseppe Tosto, MD, PhD |
Mild cognitive impairment (MCI) is a long-recognized risk factor for dementia, therefore, estimating MCI prevalence and its associated sociodemographic and health factors is critical. In collaboration with Taub colleagues Miguel Arce RenterÃa and Jennifer J. Manly, as well as collaborators from the University of Texas Medical Center, we aimed to estimate the prevalence of late-life MCI and the impact of midlife cardiovascular risk factors on MCI using a sample of 1,807 non-demented adults over the age of 55 from the Mexican Health and Age Study (MHAS).
MHAS consists of a nationally representative sample of Mexican adults aged ≥50 collected since 2001 and designed to prospectively evaluate the impact of disease on health, function, and mortality. In 2016, MHAS launched an Ancillary Study on Cognitive Aging in Mexico (Mex-Cog), a detailed and comprehensive cognitive assessment among a representative sub-sample of MHAS participants. The Mex-Cog study thus provided a unique opportunity to estimate MCI in a large sample of Mexican adults with over 15 years of follow-up.
MCI diagnosis was assigned based on a comprehensive cognitive assessment and cognitive impairment was defined by a 1.5-SD cut-off using normative corrections for age, years of education, and sex. As recently reported in the Journal of the International Neuropsychological Society, the prevalence of amnestic MCI was 5.9%. MCI was associated with older age (OR = 1.03 [1.01, 1.04], residing in rural areas (OR = 1.49 [1.08, 2.06]), depression (OR = 1.07 [1.02, 1.12]), diabetes (OR = 1.37 [1.03, 1.82]), and years of education (OR = 0.94 [0.91, 0.97]). We also found that cardiovascular risk factors in midlife increased the odds of MCI in late-life (OR = 1.76 [1.19, 2.59]. Understanding the prevalence and factors associated with MCI can help elucidate the determinants of MCI and subsequent dementia to inform research and policy for preventative strategies.
Sandra Barral, PhD
Associate Professor of Neurogenetics (in Neurology, the Gertrude H. Sergievsky Center, and the Taub Institute) at CUIMC
smb2174@cumc.columbia.edu
Giuseppe Tosto, MD, PhD
Assistant Professor of Neurology (in the Taub Institute and the Sergievsky Center)
gt2260@cumc.columbia.edu
 |
| Yaakov Stern, PhD |
There is evidence to suggest that a higher level of physical activity and high cardiorespiratory fitness (CRF) may mitigate age-related alterations in the white matter microstructure (WMM) of older adults. There is, however, a noticeable gap in the literature assessing the benefit of physical exercise training on the brain and cognition due to a lack of studies on young to middle-aged adults.
With the present study, we aimed to fill that void using previously collected data, including diffusion tensor imaging (DTI) data such as fractional anisotropy (FA) and mean diffusivity (MD), from a completed randomized clinical trial. In this RCT, 132 healthy adults aged 20–67 with below-median CRF (assessed by graded exercise test) were randomly assigned to either a supervised 6-month aerobic exercise (AE) program or a stretching/toning program. The goal was to evaluate the impact of an AE program on the WMM in a sample of young and middle-aged adults.
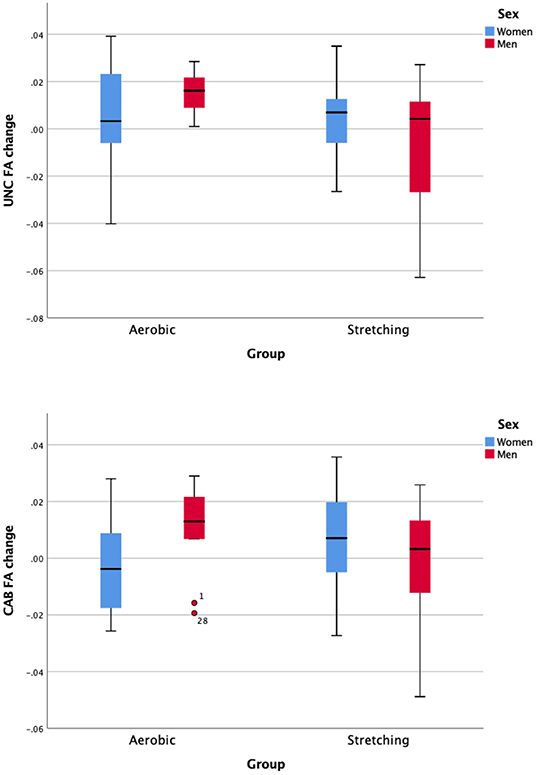
Figure 2. Sex-difference of the intervention effect in terms of change on the white matter tract fractional anisotropy of the uncinate fasciculus (UNC) and the Cingulum—angular (infracallosal) and bundle (CAB).
In a previous assessment of this RCT, we found potential sex moderation on exercise-related changes in executive function (EF), such that in any age range, men (in the AE group) improved more on EF than women. Thus, sex was included as a covariate for all analyses in this study, in an effort to examine improvement of WMM integrity as a possible mechanism by which men obtained greater cognitive benefits from AE training than women.
As recently reported in Frontiers in Human Neuroscience, no significant group-level change in WM tract microstructure following an AE training was observed. No significant correlation was found between intervention-related percentage change in terms of WMM, CRF, and cognitive performance. In this RCT, a lack of WMM improvement was also observed when analyzing the results by age group or biological sex. Without adjustment for multiple comparisons, an increase in FA and a decrease in mean diffusivity MD of the uncinate fasciculus were observed post-intervention in the AE group in comparison with the stretching group. In the AE group, a significant increase in CRF was measured but did not correlate with FA and MD change. Our study results are in accordance with similar studies in healthy adults that did not show significant benefit on WMM after participating in an AE program.
Yaakov Stern, PhD
Florence Irving Professor of Neuropsychology (in Neurology, in Psychiatry, in the Gertrude H. Sergievsky Center and in the Taub Institute for Research on Alzheimer's Disease and the Aging Brain) at the CUIMC
ys11@cumc.columbia.edu
Richard Sloan, PhD
Nathaniel Wharton Professor of Behavioral Medicine (in Psychiatry) at CUIMC
rps7@cumc.columbia.edu

