Columbia University
Irving Medical Center
Neurological Institute
710 West 168th Street, 3rd floor
(212) 305-1818
TaubCONNECT Research Perspective:
December 2023
 |
| Nikolaos Scarmeas, MD, MSc, PhD |
Cognitive and physical decline are both indicators of aging and previous research has suggested existing associations between them. Nevertheless, the underlying mechanisms of this relationship still need to be further elucidated. At the same time, it is well recognized that cerebrospinal fluid (CSF) biomarkers of Alzheimer’s disease (AD) are present in pre-clinical stages of AD. Relatively limited and often conflicting data exist regarding the relation between physical function parameters and biomarkers of the AD continuum, particularly at pre-dementia stages.
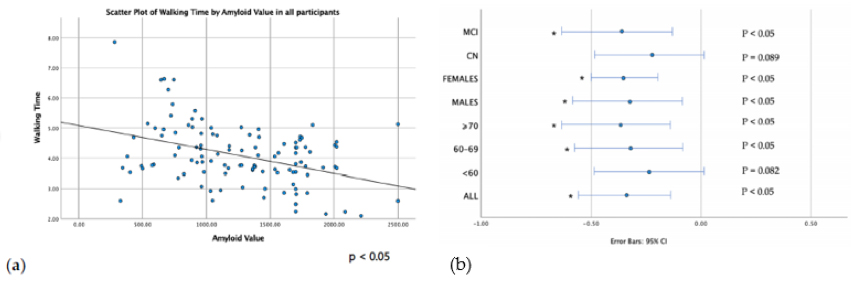
In our article published in the International Journal of Molecular Sciences, we examined the association of grip strength and walking time with AD-related CSF biomarkers using a biomarker automated method (Roche Diagnostics). Overall, 163 individuals of a broad age range (40–75 years old) of the pre-dementia AD continuum were included, with 69 % of them (n=112) being cognitively intact, and 31 % (n=51) having mild cognitive impairment (MCI). We found that walking time was inversely related to CSF amyloid Aβ42 in all participants (p<0.05), indicating slower gait in those with lower CSF amyloid (and possibly higher brain amyloid accumulation). The noted association was stronger in those with MCI, and in participants older than 60 years old, over and above adjustments for potential confounding of factors such as age, sex, education and APOE genotype.
|
Figure 1. (a) Scatter plots of linear correlation between walking time and CSF Aβ42 in all participants (b) Regression Coefficient of CSF Aβ 42 on walking time. Results are corrected for age, sex, education, years, APOE status. Associations that remained significant are indicated with an asterisk (all corrected p < 0.05)
|
In conclusion, central nervous system amyloid accumulation seems to relate to slower gait even in early stages of functional independence. Our findings can be used to further investigate whether the noted association is of causal nature as well as its detailed underlying mechanisms, especially whether amyloid accumulation influences gait performance per se or via interactions with other aspects of neurodegeneration or other neurobiological mechanisms.
Nikolaos Scarmeas, MD, MSc, PhD
Associate Professor of Clinical Neurology
ns257@columbia.edu
 |  |  | ||
| Yian Gu, MD, MS, PhD | Stephanie Cosentino, PhD | Yaakov Stern, PhD |
As Alzheimer’s disease and related dementias (ADRD) become increasingly prevalent, administrative data from routine healthcare services, like Medicare claims, are more frequently used for identifying cases. Accurate dementia identification is crucial for defining patient groups, evaluating populations, managing diseases, budgeting healthcare systems, and promoting health equity. Research has extensively documented the underidentification of dementia, particularly in racially and ethnically underrepresented groups. The lack of timely diagnosis impedes early-stage disease management and treatment, support for patients and caregivers, and access to clinical trials. In contrast, overidentification of dementia, can lead to unnecessary costs for diagnosis, inappropriate disease management, and increased stress and decreased quality of life for patients, with these negative outcomes often more pronounced in minority groups.
In a study recently published in the Journal of Alzheimer’s Disease, Drs. Yaakov Stern, Stephanie Cosentino, Yian Gu, and colleagues investigated the extent and variation of dementia misidentification in the ethnically diverse Washington Heights-Inwood Columbia Aging Project (WHICAP) cohort. The investigators compared ICD-9-CM and ICD-10-CM codes from Medicare claims (1999–2019) with the clinical dementia diagnosis, and with the association between race (White, African American/Black, other) and ethnicity (Hispanic/Latinx, non-Hispanic/Latinx) and dementia identification accuracy, factoring in clinical and demographic details, as well as hospital and outpatient visits. They found that 88.4% showed accurate dementia identification when matched with the clinical diagnosis, 4.1% were wrongly labeled as having dementia, and 7.5% were not identified when they should have been. African American/Black participants had a 2.2% higher chance of being inaccurately identified as having dementia compared to White participants, and Hispanic individuals had a 2.7% higher likelihood than non-Hispanics.
This study by Zhu et al. underscores the persistent racial and ethnic disparities in the misdiagnosis of dementia. It reveals that Black and especially Hispanic older adults face a higher likelihood of both underdiagnosis and overdiagnosis of dementia compared to their White peers. These findings suggest that individuals from these minority groups could significantly benefit from more precise and thorough dementia assessments to prevent misdiagnosis. There is a clear need for increased efforts to comprehend and minimize these disparities in dementia identification.
Yaakov Stern, PhD
Florence Irving Professor of Neuropsychology (in Neurology, Psychiatry, the Sergievsky Center, and Taub Institute)
ys11@cumc.columbia.edu
 |  | |
| Stephanie Cosentino, PhD | Yian Gu, MD, MS, PhD | |
|  | |
| Davangere P. Devanand, MBBS, MD | Yaakov Stern, PhD |
As the U.S. population ages and becomes increasingly diverse in terms of race and ethnicity, it becomes crucial to gain a deeper understanding of the factors that influence the varying progression of Alzheimer's disease (AD) across different populations. This knowledge is essential for improving patient care and for the creation of more effective treatment strategies tailored to diverse groups.
Neuropsychiatric symptoms (NPS), such as hallucinations, delusions, agitation, aggression, and depression, frequently occur in AD patients. Previous research by Dr. Yaakov Stern found NPS to be linked to more severe outcomes like accelerated disease progression. In the current study, Dr. Stern and colleagues, including Drs. Davangere Devanand, Yian Gu, and Stephanie Cosentino, examined the relationship between NPS and cognitive function, as well as level of dependency, in a diverse group of community dwelling older adults from the Predictors 3 research study. Among 293 participants, 138 were identified with probable AD at the beginning of the study.
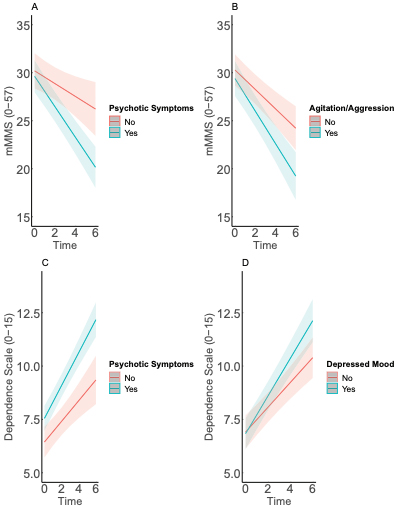
Figure 2. Predicted trajectories over 6 years of follow-up for adjusted mixed-effects models (n=138). Plot “A” depicts model predicted trajectories for cognition by psychotic symptoms. Plot “B” depicts model predicted trajectories for cognition by agitation/aggression. Plot “C” depicts model predicted trajectories for dependence by psychotic symptoms. Plot “D” depicts model predicted trajectories for dependence by depressed mood. Predicted trajectories calculated for Hispanic females, 86 years old, with 5 years of education, clinical dementia rating score of 1, no Apolipoprotein E-ϵ4 polymorphism, and 3 or more comorbidities. Shaded areas represent 95% confidence bands.
As recently reported in Current Alzheimer Research, they found that psychotic symptoms are linked to an accelerated increase in dependence and a decrease in cognitive functions over time. Specifically, agitation/aggression was connected to a quicker decline in cognitive abilities, while depressed mood was associated with a rapid increase in dependence. Notably, among psychotic symptoms, delusions (but not hallucinations or illusions) were linked to poorer outcomes. Furthermore, depressed mood was observed to significantly increase dependence in males, but this was not evident in females. These findings contribute to the expanding literature on factors that influence AD progression, particularly in community-based groups that more accurately represent the diverse aging demographic in the U.S.
Yaakov Stern, PhD
Florence Irving Professor of Neuropsychology (in Neurology, Psychiatry, the Sergievsky Center, and Taub Institute)
ys11@cumc.columbia.edu
Effects of Lithium on Serum Brain-Derived Neurotrophic Factor in Alzheimer's Patients with Agitation
 |
| Davangere P. Devanand, MBBS, MD |
Brain-derived neurotrophic factor (BDNF) plays an important role in neuronal survival and growth, serves as a neurotransmitter modulator, and participates in neuronal plasticity, which is essential for learning and memory. There is ample evidence in animal models that lithium increases BDNF levels, but human studies on the effects of lithium on BDNF are limited. In one study of patients with Mild Cognitive Impairment, serum BDNF increased after treatment with lithium. In an NIA-funded, randomized, placebo-controlled clinical trial of low-dose lithium to treat agitation in Alzheimer’s disease that was led by Taub faculty member Dr. D.P. Devanand at the New York State Psychiatric Institute and Columbia University, serum levels of BDNF prior to and after the 12-week randomized placebo-controlled trial were assessed. In this report with co-authors Jamie Graff and Deborah Deliyannides, published in the International Journal of Geriatric Psychiatry, BDNF levels did not change significantly during the trial and were not associated with improvement in overall neuropsychiatric symptoms or in cognitive function. More research is needed to understand the potential effects of lithium on BDNF in AD and whether the effects are dependent on the stage of cognitive decline and dementia.
Davangere P. Devanand, MBBS, MD
Professor of Psychiatry (in Neurology and in the Gertrude H. Sergievsky Center) at the CUMC
dpd3@cumc.columbia.edu